Boost Patient Retention with Chronic Care Management
Patient retention is more than keeping appointments; it builds trust, cultivates long-term relationships, and delivers sustainable care. For patients with chronic diseases, staying engaged in their healthcare journey is critical for improved outcomes and overall well-being. How do healthcare professionals ensure that patients remain committed to their care plans?
The answer lies in Chronic Care Management (CCM). Through active management of patient’s health, customized support, and technology, providers can enhance engagement, satisfaction, and retention. Here’s how CCM can convert patient loyalty into a long-term commitment and improve patient outcomes.
How Chronic Care Management Increases Patient Retention
Proactive Engagement : Staying Connected Beyond Meetings
Patients appreciate being taken care of even when they are not in their scheduled appointments. Regular check-ins via phone, text, or telehealth underscore their importance to your practice. Whether it is a friendly reminder about an upcoming appointment or an informal “How are you today? these check-ins build trust and make it more likely patients will stay engaged.
Individualized Care Strategies : Making Sure Patients Feel Heard and Understood
Healthcare is not one-size-fits-all, and patients know that. When care plans are tailored to their individual needs, preferences, and goals, they feel valued and respected. This personal attention fosters loyalty, as patients will stick with a provider who genuinely cares about their well-being.
Effortless Collaboration : Reducing the Burden of Care Management
Many long-term condition patients coordinate multiple specialists, therapies, and medications. CCM ensures smooth coordination of healthcare professionals, eliminating guesswork and ensuring that no minute detail is missed. When patients experience easy, hassle-free care, they are far more likely to stay loyal to your practice.

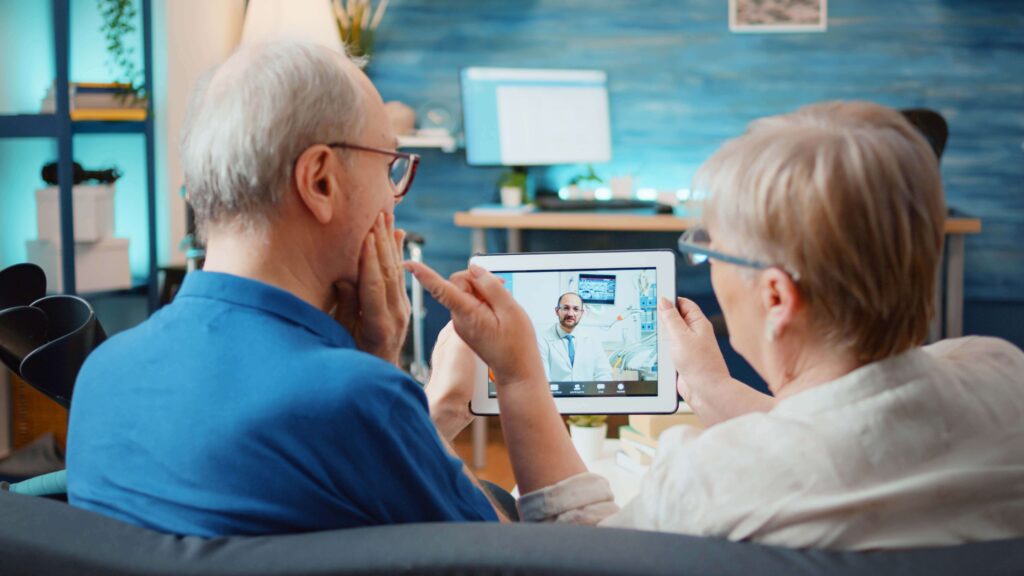
Instant Help through Remote Patient Monitoring (RPM)
Wearable gadgets and home monitoring systems enable providers to monitor essential health information instantly. This not only minimizes hospital visits but also comforts patients’ confidence that their health is being proactively managed—even remotely. When patients realize their provider is only a step ahead, they feel more secure and engaged.
Round-the-Clock Support Availability : Health Issues Don’t Adhere to Timetables
When patients know that help is available at any time whether through nurse hotlines, drug support programs, or online services they gain confidence in their healthcare provider. The assurance of immediate relief fosters long-term loyalty and minimizes the likelihood of switching providers.
Educating Patients : Empowering People to Take Charge
An educated patient is an engaged patient. Providing educational resources on chronic disease, self-care practices, and lifestyle modifications helps patients make better health decisions. When people feel more in control of their health, they are more likely to stay committed to their care plan and healthcare team.
Preventing Hospital Readmissions : Keeping Patients in the Right Place
No one wants to return to the hospital unless necessary. CCM’s proactive approach helps prevent readmissions by supporting medication compliance, monitoring symptoms, and acting early when possible issues arise. Those patients who are faced with fewer disruptions in their normal lives have a greater sense of appreciation for the care of their providers.
Addressing Social Determinants of Health: Overcoming Barriers to Access to Care
Financial challenges, transportation problems, or hunger issues may complicate the control of chronic conditions. CCM programs help bridge these gaps by connecting patients to community resources so they receive support ensuring their treatment remains continuous.
Emphasis on Mental and Emotional Health
Dealing with a chronic illness impacts mental health. Patients need more than a doctor’s care—they also want emotional support. Monthly visits, support groups, and stress reduction materials help patients feel heard and supported, making them more attached to their providers.
Improving Retention & Reducing Attrition
- Treat patients respectfully and hear them out.
- Foresee problems and setbacks before they occur.
- Keep up with appointments to reduce wait times.
- Pre-screen appointments ahead of time to eliminate no-shows.
- Call patients when visits are past due.
- Ask patients to complete surveys to solicit feedback and enhance service.
- Institute a recall system to arrange follow-up visits before departure.
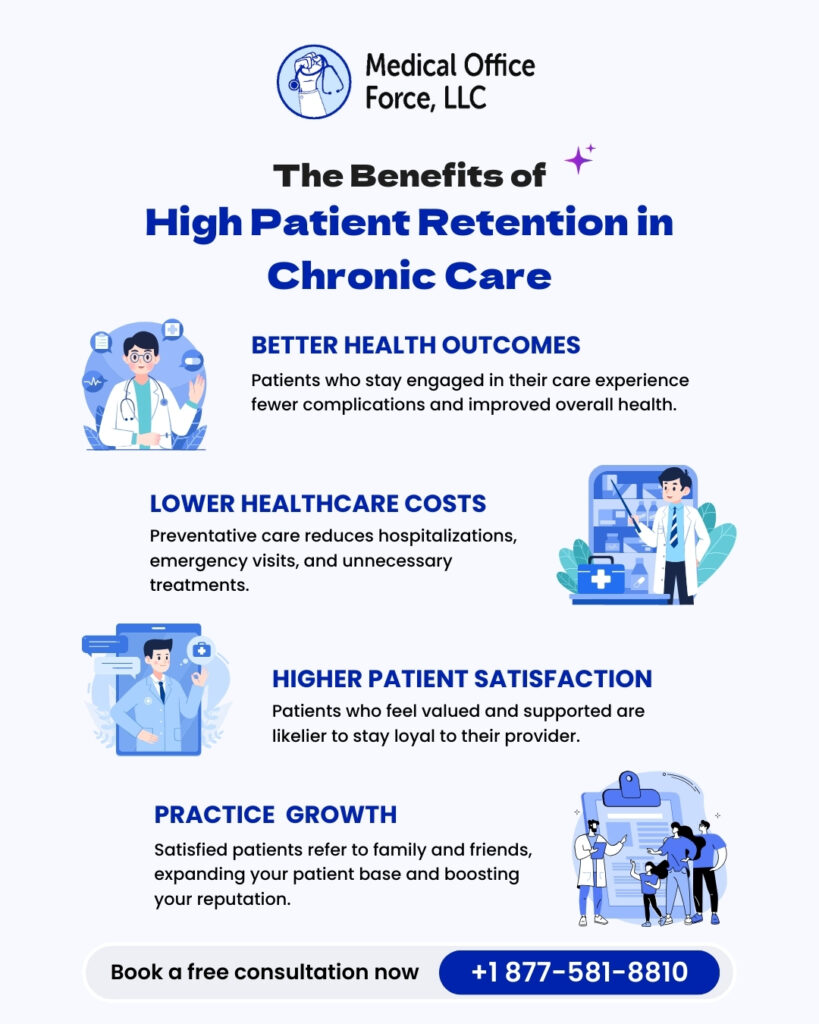
The Future of Patient Retention is Proactive Care
Patient retention isn’t about keeping patients, it’s about providing them with reasons to never want to leave. Chronic Care Management offers the framework, assistance, and proactive interaction that keeps patients engaged in their health and their healthcare provider. By investing in CCM initiatives, you’re not merely retaining patients, you’re changing lives.
Take Action Today
If you are ready to increase patient retention and better outcomes, begin implementing CCM in your practice. A well-supported patient is a loyal patient, and a loyal patient guarantees the long-term success of the healthcare organization.
What are you doing today to enhance patient engagement and retention?