
Denial Management in Healthcare
Medical billing is a complex system, in which, denial management represents enormous financial and operational hurdles. Claim denials are an ongoing challenge that puts an on healthcare providers’ finances and administrative workloads. These denied claims may result in lost income and revenue cycle inefficiencies if a robust denial management plan is not implemented.
The Medical Group Management Association (MGMA) states that claim denials are manageable and recoverable under comprehensive and sufficiently aggressive processes. This blog will discuss the denial management processes, frequently occurring reasons for claim denial, the best denial management practices, and how optimally handled denial management can contribute towards revenue.
What Can Denial Management Do?
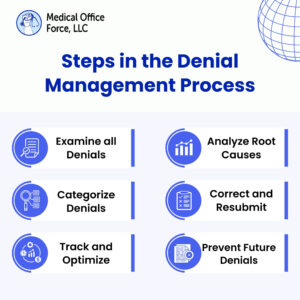
Denial management services within the healthcare setting refer to identifying, resolving, and taking measures to prevent claim denials to achieve maximum reimbursement. It includes studying denied claims to search for patterns, correcting the mistakes, and taking steps to prevent similar denials in the future.
Why Is Denial Management Important?
- 1. Optimizes revenue cycle processes and improves the cash flow of the facility
- 2. Reduces the administrative workload that reprocessing claims creates
- 3. Improves relations between a payer and a provider
- 4. Increases patient satisfaction by improving billing concerns and issues.
Increases patient satisfaction by improving billing concerns and issues Common Reasons for Denied Claims:
1. Timely filing of claims: Claims submitted after the payers’ deadline are automatically denied.
2. Subscriber Identification: Mismatched patient information leads to rejection.
3. Services : Services not covered under the patient’s insurance plan.
4. Bundled Services: Incorrect bundling of services may lead to denials.
5. Incorrect use of modifiers: Improper use of coding modifiers can trigger denials.
6. Discrepancies in Data: Inconsistent or missing data results in claim rejection
How Does Denial Management Contribute to Revenue Optimization?
Effective denial management minimizes revenue loss and accelerates reimbursements. On identifying and rectifying denied claims, practices can:
1. Maximize revenue potential
2. Improve cash flow stability
3. Reduce administrative costs.
4. Enhance overall financial performance
At Medical Office Force, we specialize in denial management services, providing expert solutions to help medical practices streamline operations, reduce claim denials, and optimize revenue.

Key Performance Indicators (KPIs) for Denial Management
Monitoring KPIs helps assess the effectiveness of denial management efforts:
1. Denial Rate : Percentage of claims denied by payers.
2. Denial Reasons : Identification of common denial causes.
3. Days in Accounts Receivable (AR) : Time taken to collect payments.
4.Denial Resolution Turnaround Time: Speed of resolving denied claims.
5. Denial Appeal Success Rate: Percentage of successfully appealed denials.
How Can Claim Denials Be Minimized With A Better Medical Practice?
Claim denials are best dealt with by using an efficient approach. Claim errors that result in denied claims and are costly can be mitigated by adopting effective preset approaches.
1. Patient Registration: Record insurance and patient details accurately.
2. Documentation: Omitting coding mistakes requires detailed and accurate medical documentation.
3. Staff Training: Coding and billing mistakes diminish with regular education on updates.
4. Submission of Claims: Claims are submitted on time to avoid denial due to late filing.
5. Regular Audits: Review submission aids in identifying mistakes that harm claims.
What Comes After A Claim Has Been Denied?
Minimizing any potential loss that can come from a denied claim can be handled by:
1. Timely Action: Make use of all documentation that can help to prove the claim.
2. Review the Denial Reason: Investigate the claim reimbursement and reason for denial.
3. Gather Necessary Documentation: Compiling all necessary evidence to support the claim.
4. Decide if A Reasonable Appeal Needs To Be Made: If any strong evidence does not back the denial, consider the claim appeal process, as some claim denials can be eliminated through an appeal.
5. Quick Action: To increase the likelihood of making a successful appeal, do so within the deadlines provided.
Two-thirds of rejected claims are recoverable according to the Journal of AHIMA. Denial management supports revenue recovery which is imperative and should be effortless to manage.
Best Practices in Denial Management
To reduce denials and improve efficiency, the following best practices can be considered:
-Maintaining detailed records and documentation
-Regular analysis of denial trends and metrics.
-Avoiding backlogs by immediately addressing denials.
-Implementing preventive strategies by monitoring common reasons for denials.
-Assigning a dedicated team for denial management.
-Utilizing advanced software for tracking and resubmitting claims.
-Maintaining open communication with insurance providers.
-Monitoring key performance indicators (KPIs) for continuous improvement.
-Avoid bulk submissions and prioritize accurate claims
-Regularly auditing the process to avoid gaps
-Avoiding mistakes made in previous denials
-Verifying insurance verification thoroughly before service
-Hold on to payer submission and appeal deadlines
-Keeping track of pending and appealed claims.

Conclusion
Denial control in healthcare is not just about fixing mistakes, it’s about preventing them. Medical practices can substantially reduce denials and improve financial stability by implementing robust strategies, bringing in automation, and staying proactive.
At Medical Office Force, we assist healthcare providers in streamlining their denial control procedure, making sure quicker reimbursements and reduced revenue loss.
Contact us today to learn more about our denial control offerings and the way we will help optimize your revenue cycle. Transform your practice’s monetary health with effective denial control!
Resources:
https://www.ahima.org/
https://www.cleveland.com/
https://www.nih.gov/
https://www.mayoclinic.org/

